Psoriasis Awareness Week Archive
2020's event ran from Thursday 29th October (World Psoriasis Day) to Wednesday 4th November.
 Please use the links below to navigate to the relevant section.
Please use the links below to navigate to the relevant section.
- About
- Please still write to your MP and help us raise awareness of psoriasis in Parliament
- Plaque psoriasis - Thursday 29th October
- Scalp psoriasis - Friday 30th October
- Guttate psoriasis - Monday 2nd November
- Pustular psoriasis - Tuesday 3rd November
- Psoriatic arthritis and nail psoriasis - Wednesday 4th November
- More types of psoriasis
- 'Psoriasis, COVID-19 and Me' - FREE webinar
About
Psoriasis Awareness Week runs annually and aims to raise awareness of psoriasis and psoriatic arthritis. 2020's theme was different types of psoriasis.
Did you know that psoriasis can take several different forms? For Psoriasis Awareness Week 2020, we took a closer look at the types of psoriasis which we are most commonly asked about on our helpline, the ways in which they are treated, and the impact they can have on people's lives.
Read on below to find out more about the different types of psoriasis, discover real life stories from the people who are living with them, and get tips from the experts.
Please still write to your MP and help us raise awareness of psoriasis in Parliament
We're still very keen to raise awareness of psoriasis in Parliament, so please do still write to your MP!
 Sir Edward Leigh MP, the Chair of the All Party Parliamentary Group on Skin, kindly agreed to host an Early Day Motion (EDM) in Parliament which recognises the vital work of the Psoriasis Association and calls upon the Government to investigate ways to improve access to all relevant healthcare professionals for people with psoriasis whose essential treatment has been unfairly delayed by the impact of the COVID-19 pandemic.
Sir Edward Leigh MP, the Chair of the All Party Parliamentary Group on Skin, kindly agreed to host an Early Day Motion (EDM) in Parliament which recognises the vital work of the Psoriasis Association and calls upon the Government to investigate ways to improve access to all relevant healthcare professionals for people with psoriasis whose essential treatment has been unfairly delayed by the impact of the COVID-19 pandemic.
We need as many parliamentary representatives as possible to get involved, so please do contact your local MP and to ask them to sign EDM #1049.
You can read the text of the Early Day Motion or see whether your local MP has already signed it here.
You can find out who your local MP is here.
You may also want to tweet your MP (Find out if they have a Twitter handle here.) A suggested tweet could be:
@[MPNAME] - Please support EDM 1049 which asks the Government to improve access to all relevant healthcare professionals for people with #psoriasis during the COVID-19 pandemic https://edm.parliament.uk/early-day-motion/57613
Please do write to your local MP and tell them about the issues you have faced with psoriasis. We have also put together a template letter which you can download, personalise and send to your MP.
It will be great to get as many MPs signing the EDM as possible to help raise awareness of psoriasis and psoriatic arthritis. The more MPs that are aware they have a constituent with psoriasis, the more weight will be added further down the political line.
Plaque psoriasis – Thursday 29th October
On Thursday 29th October (World Psoriasis Day),
we kicked off Psoriasis Awareness Week by focusing on plaque psoriasis – the
most common form of psoriasis.
Most people with psoriasis have plaque psoriasis, either alone or in combination with another type. It gets its name from the ‘plaques’ that are formed by the build-up of skin cells. These can be very red, itchy and sore, with white or silvery scales.
As well as providing more information about plaque psoriasis and sharing a plaque psoriasis Q&A with Emma, psoriasis experts Professor Chris Griffiths and Dr Helen Young answered some of the questions you submitted during the recent psoriasis Priority Setting Partnership (PSP) exercise.
Professor Chris Griffiths - Answering your psoriasis questions
Professor Griffiths is Professor of Dermatology at the University of Manchester, Honorary Consultant Dermatologist at Salford Royal NHS Foundation Trust and co-investigator on the psoriasis Priority Setting Partnership (PSP). In the video below, he answers the following questions:
- What is psoriasis? (0:09)
- What are the different types of psoriasis and what do they have in common / how do they differ? (1:02)
- At what age can psoriasis develop? (2:57)
- Can you experience more than one type of psoriasis at one time? (3:55)
- What research is currently being done into psoriasis? (4:39)
- What are the main treatments/drugs used in the treatment of psoriasis? (1:02)
- What is the first line treatment for psoriasis? (1:51)
- Why are biologic injections only being given to people who have had side effects from other immunosuppressant drugs, or when the immunosuppressant drugs haven’t worked? (2:43)
- What new treatments are on the way? (3:51)
- How does plaque psoriasis affect you? (0:00)
- How do you manage your plaque psoriasis? (00:51)
- What do you wish other people knew about living with plaque psoriasis? (1:47)
- What advice would you give to someone who has just been diagnosed with plaque psoriasis? (2:41)
Dr Helen Young - Answering your psoriasis treatment questions
Dr Young is a Senior Lecturer in Dermatology at the University of Manchester and Consultant Dermatologist at Salford Royal NHS Foundation Trust. She was also the Lead Investigator for the psoriasis Priority Setting Partnership (PSP). In the video below she answers the following questions:
Plaque psoriasis Q&A with Emma
In the short video below, Emma shares her experiences of life with plaque psoriasis. She answers the following questions:
Scalp psoriasis – Friday 30th October
Friday 30th October saw us move our focus to
scalp
psoriasis. The scalp is one of the areas of the body which is most commonly
affected by psoriasis.
Scalp psoriasis usually involves a thick build-up of plaques of skin, which may cause dandruff-like flakes to fall. It may also be visible around the hairline, on the forehead, neck and behind the ears. It can make the scalp feel itchy and tight, and severe cases can cause temporary thinning of the hair, which can be resolved with effective treatment of the psoriasis.
Below you can find our brand new scalp psoriasis tips resource, and a scalp psoriasis Q&A with Michelle too.
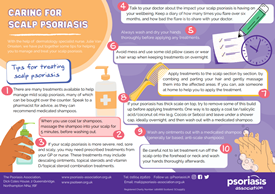
Scalp psoriasis tips resource launched
On the second day of Psoriasis Awareness Week, we focused on scalp psoriasis. Scalp psoriasis is one of the topics we are most commonly asked about on our helpline.
Scalp psoriasis can be persistent, itchy and uncomfortable, while trying to treat the scalp through the hair can be tricky. There are many different treatment options available but finding the right one can be a process of trial and error.
With the help of dermatology specialist nurse, Julie Van Onselen, we've put together some tips to help you manage and treat your scalp psoriasis.
There are pointers for caring for your scalp, tips for applying treatments to the scalp, and also some handy suggestions for trips to the hairdresser too.
You can download a copy of the resource here
Michelle - Scalp psoriasis Q&A
Michelle takes part in a Q&A for Psoriasis Awareness Week 2020 to share her experiences of scalp psoriasis.
The Q&A covers the following questions:
- When were you first diagnosed with scalp psoriasis?
- How does your scalp psoriasis affect you?
- How do you treat/manage your scalp psoriasis?
- What do you wish other people knew about living with scalp psoriasis?
- What advice would you give to someone who has just been diagnosed, or suspects they might have scalp psoriasis?
Guttate psoriasis – Monday 2nd November
On Monday 2nd November we put the spotlight on guttate
psoriasis – a type of psoriasis which is particularly common in
children, teenagers and younger adults.
Guttate psoriasis is also known as ‘tear drop’ or ‘rain drop’ psoriasis because of its appearance. Guttate spots are often a bright pink or red on fair skin types, whilst people with darker skin types may notice less reddening and more darkening. There may also be some fine scaling on guttate spots.
Guttate psoriasis is usually widespread across the torso, back and limbs, and clears up after several weeks or months. It is often triggered by a streptococcal throat infection.
Below you can watch a guttate psoriasis Q&A with Consultant Dermatologist, Dr Julia Schofield and read Anne's guttate psoriasis story.
Dr Julia Schofield - Answering your guttate psoriasis questions
Dr Julia Schofield is Vice-Chair of the Psoriasis Association and a Consultant Dermatologist at United Lincolnshire Hospitals NHS Trust. In the video below she answers the following questions about guttate psoriasis.
- I’ve been advised to get the flu jab but I have had a flare up of guttate psoriasis in the past after having it and was advised never to have it again. Is the advice still the same? (1:02)
- What would be the best topical treatment for guttate (given the widespread nature of it, and the restrictions of not getting strong steroids / tar onto healthy skin)? (2:09)
- Because tonsillitis often precedes guttate psoriasis, how do I take swift action to prevent a flare from getting too bad? Would it help to have my tonsils removed? (3:13)
- How do I access phototherapy swiftly as the waiting times may be longer than the guttate flare (in some areas)? Should I get a sunbed to treat my guttate psoriasis? (5:40)
- Who is most likely to get guttate psoriasis, and will it always mean you go on to get plaque psoriasis afterwards? (7:04)
- Can guttate psoriasis spread to the face and if it can, how should it be treated? (7:44)
- What are the treatment options for guttate psoriasis? (8:52)
- What triggers guttate psoriasis? (10:34)
- How long does a flare of guttate psoriasis normally last? (11:31)
Anne, now 55, was first diagnosed with guttate psoriasis at 3 years old and is sharing her story for Psoriasis Awareness Week 2020.
From diagnosis to school days, treatment choices to clothing choices, Anne explains how her psoriasis has impacted many different parts of her life.
With the help of an effective treatment her psoriasis is now much better controlled and she is keen to let others know about the supportive psoriasis community on social media.
Pustular psoriasis – Tuesday 3rd November
Pustular
psoriasis was our focus on Tuesday 3rd November. This
is a kind of psoriasis where small white or yellow blisters (pustules) appear
on top of very red or darkened skin.
There are two different types of pustular psoriasis: Palmoplantar Pustulosis (PPP), which affects only the palms of the hands and/or soles of the feet; and Generalised Pustular Psoriasis (GPP) which looks similar to PPP but is usually widespread across the body, rather than confined to a particular area.
Both types of pustular psoriasis can be painful and – particularly when the palms of the hands and soles of the feet are affected – can make walking and other everyday activities difficult.
Below you will find a Q&A with Psoriasis Association-funded researcher, Dr Francesca Capon, who explains more about her team's important research into pustular psoriasis. You can also read Linzi's pustular psoriasis story too.
Dr Francesca Capon - Discovering the mechanisms behind pustular psoriasis
Dr Francesca Capon is a Reader in Inflammation Genetics at King's College London. In the video below, she answers questions about her Psoriasis Association funded research project: Characterisation of Novel Pathogenic Pathways for Generalised Pustular Psoriasis.
Questions covered in the video include:
- What was the aim of the project? (0:31)
- What did you discover? (1:40)
- Why are these results important? (3:10)
- Is there any current work building on these results? (4:04)
- How can people find out more about your work? (5:06)
Although Linzi first developed psoriasis more than 10 years ago, it was a few years later before she had a first flare up of pustular psoriasis.
After several trips to her GP, she received a diagnosis of pustular psoriasis from a dermatologist and was soon admitted to the dermatology ward at her local hospital for inpatient treatment.
Five years on, and having tried a variety of different treatments along the way, Linzi is in a much better place with her skin and is keen to share her experiences for Psoriasis Awareness Week 2020.
Psoriatic arthritis and nail psoriasis – Wednesday 4th November
On the final day of Psoriasis Awareness Week, we looked
at psoriatic
arthritis – an inflammatory arthritis which is associated with
psoriasis – and nail
psoriasis, which affects up to 50% of all people with psoriasis and
up to 80% of people with psoriatic arthritis.
Psoriatic arthritis (PsA) affects joints (such as the knees or those in the hands and feet), as well as areas where tendons join to bone (such as the heel and lower back). Most people who develop psoriatic arthritis find it occurs after developing psoriasis on their skin, but some develop the arthritis before they notice any symptoms of psoriasis.
Nail psoriasis can affect either the fingernails or toenails, or both. It is possible for a person to just have psoriasis of the nails, with no other symptoms of psoriasis on the skin. Symptoms of nail psoriasis can include discolouration of the nail, ‘pitting’ (small dents) across the surface of the nail, nails that split or crumble easily, thickening of the nail, and nails that lift or detach themselves from the nail bed (onycholosis).
Below, Consultant Rheumatologist, Professor Laura Coates provides an update on the Psoriatic Arthritis Priority Setting Partnership – an exercise to help find the ‘Top 10’ questions that future psoriatic arthritis research should address.
You can also read Joel's psoriatic arthritis story, and Liz's nail psoriasis story too.
Professor Laura Coates - Setting priorities in psoriatic arthritis research
Earlier in 2020 the psoriatic arthritis Priority Setting Partnership (PSP) was launched in order to identify the top 10 unanswered questions that people who are living with the condition as well as their families, carers and clinicians would most like future research to address.
We're delighted to bring you an update from the Lead Investigator on this project, Consultant Rheumatologist, Professor Laura Coates, in the video below, where she answers the following questions:
- Who do you see in your clinic? (0:21)
- What does your research involve? (2:42)
- What is the psoriatic arthritis Priority Setting Partnership? (3:20)
- What will this research achieve? (5:26)
Joel first developed psoriatic arthritis in his twenties and now blogs in order to record his personal experiences.
He credits the supportive arthritis community for helping him find his voice and start his blog, and his since written for a number of charities and organisations, including the Psoriasis Association.
This Psoriasis Awareness Week, Joel is keen to share his story and help reassure others who may be going through a journey similar to his own.
Liz has been living with the symptoms of nail psoriasis for the past two and a half years, but only received a diagnosis earlier this year.
Since that point, she has tried a number of different treatments and found ways to manage her nails to stop them catching and causing her pain when going about her day-to-day life.
Liz has kindly agreed to share her experiences as part of our #KnowYourPso campaign for Psoriasis Awareness Week 2020.
More types of psoriasis
We
have chosen specifically to feature the five types of psoriasis mentioned above
because they are the types that we are most frequently asked about on our
helpline. However, there are other types of psoriasis too, including facial
psoriasis and late onset psoriasis.
Facial psoriasis
Facial psoriasis may be less clearly-defined than psoriasis elsewhere on the body. The face is a sensitive area which means that not all treatments which are used for psoriasis on other areas of the body are appropriate for use on the face. Psoriasis on the face can also be very visible and difficult to cover. As such, it can have a particular impact on a person’s quality of life.
Aimee – Facial psoriasis
For Psoriasis Awareness Week 2020, Aimee has kindly agreed to share her experiences of facial psoriasis and how she has learned to love her skin.
Despite living with different types of psoriasis since she was 14, Aimee first developed facial psoriasis in her early 30s and has found it the most difficult to come to terms with due to its visible nature.
Nonetheless, Aimee has embraced her psoriasis and is now keen to set a positive example for others to follow.
Read Aimee’s story here
Late onset psoriasis
While psoriasis can occur at any age, there seem to be two ‘peaks’: the first from the late teens to early 30s (early onset psoriasis); and the second between the ages of around 50 to 60 (late onset psoriasis).
While both are roughly as common as each other, late onset psoriasis does not tend to be discussed as much, but it’s important to be aware that psoriasis can develop later in life too.
Jonathan – Late onset psoriasis
For this year’s Psoriasis Awareness Week, Jonathan has agreed to share his experiences of late onset psoriasis, having first developed the condition at the age of 60. Watch the video below to hear his story.
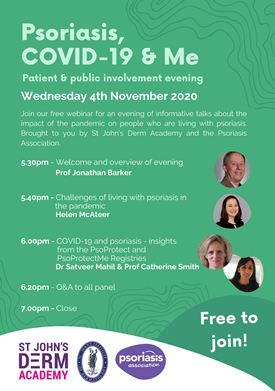
'Psoriasis, COVID-19 and Me' - FREE webinar
The Psoriasis Association was delighted to team up with St John's Derm Academy to have brought you ‘Psoriasis, COVID-19 and Me’, an online evening of informative talks about the impact of the pandemic on people who are living with psoriasis.
The webinar featured discussion from psoriasis experts Prof. Jonathan Barker, Prof. Catherine Smith and Dr Satveer Mahil. Our Chief Executive, Helen McAteer, also spoke about some of the challenges of living with psoriasis during the pandemic.
During the evening, attendees heard new insights from PsoProtect and PsoProtectMe, the registries behind vital research into COVID-19 and psoriasis. There was also the opportunity to ask the expert panel questions in the Q&A session which followed.
We are keen to share the sessions from the webinar with a wider audience after the event, so watch this space! We will also be doing our best to make the Q&A session available, along with written answers to any questions that the panel didn't have time to answer on the night.
Many thanks to the presenters, panel and everyone who attended for making this such a successful event!